In the two previous chapters I outlined the key science underpinning skin cancer susceptibility. UVR damages DNA, but DNA repair is imperfect and therefore mutations accumulate. Melanin acts to protect against this process.
If we now add in some ‘common sense’ facts we can build a complex map of susceptibility that guides our clinical behaviour. We can, to use the cliché, move from bench to clinic. Let us see how these predictions work out.
This chapter in one minute
Age
Age is a proxy for exposure to UVR in that, on average, older people will have had more UVR exposure — simply because they have been on this earth longer. Older people will therefore have accumulated more mutations.
We therefore expect skin cancer rates to rise with age — which is, of course, what we do see. It is not therefore the ‘age of the patient per se‘, but merely the fact that age is a marker of cumulative UVR exposure (and damage).
Ambient exposure to UVR
If UVR is the main cause of UVR, then the epidemiology of skin cancer must be strongly influenced by the patterns of exposure to UVR. This will include ambient UVR, and the relation between different body sites and ambient UVR.
Image on left: Australia_(orthographic_projection).svg, CC BY-SA 3.0, Link
People living in areas with high ambient UVR will — all other factors being equal — have higher skin cancer rates. We therefore expect skin cancer rates to be higher in those living close to the equator. We can unpack this further. If people migrate to a sunny climate later in life, their childhood exposure will likely have been less, and therefore their rates may remain lower than those born and brought up in their adopted land.
Whatever the ambient UVR, different body sites are exposed differently. The scalps of bald headed men, the backs of the hands, and the tops of the ears receive more UVR than the buttocks, the back or the legs.
There are some details that may not be obvious. Traditionally, the tops of the ears of men receive much more UVR than the equivalent area of women — hair is more likely to cover the ears in women than men. Therefore, in some populations, we see melanoma rates that are 3-5 times higher in men than women on the tops of the ears. If the fashion for some young men to shave their scalp continues, you can work out what might happen. Those ageing hippies with their long hair were perhaps onto something…..
Human behaviour
Although the amount of ambient UVR is one factor, individual behaviour in the sun is also critical. Do you spend much time at the beach ?
The more clothes that are worn, the lower the UVR dose the skin receives. If you are bald, but wear a hat, the effective UVR dose is diminished. If you have hobbies, or work in an occupation that increases exposure (e.g. surfing, fishermen), your UVR exposure is increased.
Again, the permutations may not be obvious. There is indeed more UVR in Brisbane than Glasgow, but a child addicted to computer games in Brisbane may receive less UVR than a child in Glasgow who spends much of their leisure time playing football.
Pigmentary phenotype
The previous chapter highlighted how important melanin pigmentation is in preventing against UVR damage and skin cancer. The more eumelanin there is, the more protected skin is. Dark skinned Africans are over 100 times less at risk of developing skin cancer than pale skinned North Europeans.
But there remain some gaps in our knowledge of pigmentation and skin cancer risk. Those with red hair, for instance, tend to have paler skin that those without red hair. Their skin also tends to have less eumelanin, and possibly more pheomelanin either in absolute terms or in relative terms (their hair certainly has a higher absolute amounts of pheomelanin, than those with blonde or dark hair).
There is however still debate about whether it is the absence of eumelanin that is the chief problem, or whether pheomelanin is not only not very protective, but positively harmful if exposed to UVR. Whatever the exact mechanism, those with red hair or those with a phenotype characterised by more pheomelanin in their hair, are at increased risk of skin cancer. This phenotype is characterised by not only red hair, but abundant freckles (focal areas of overproduction of melanin). Freckles reflect both UVR exposure and the underlying pigmentary phenotype.
Freckles are a marker of both genes and environment (sun exposure)
Images with permission of Reto Caduff. Link.
Genetics: Mendelian
We have mentioned the contribution of genetics on several occasions. Xeroderma pigmentosum is an autosomal inherited disorder characterised by an inability to repair UVR induced DNA damage, so cancer rates are increased. Albinism is a group of (autosomal recessive) inherited disorders characterised by a reduction in the amount of melanin, leading to increased cancer rates. The clinical phenotype of albinism will of course reflect the type of albinism and UVR exposure: an albino living on the equator will more likely come to harm than one living in Finland.
And, as just discussed, those with red hair, a trait under the control of the melanocortin 1 receptor (OMIM #155555), which approximates to a Mendelian recessive trait, are at a 3-5 fold increased risk of skin cancer.
There is one other group of Mendelian disorders, that we have not mentioned already, but we which need to briefly highlight: inherited tumour suppressor syndromes.
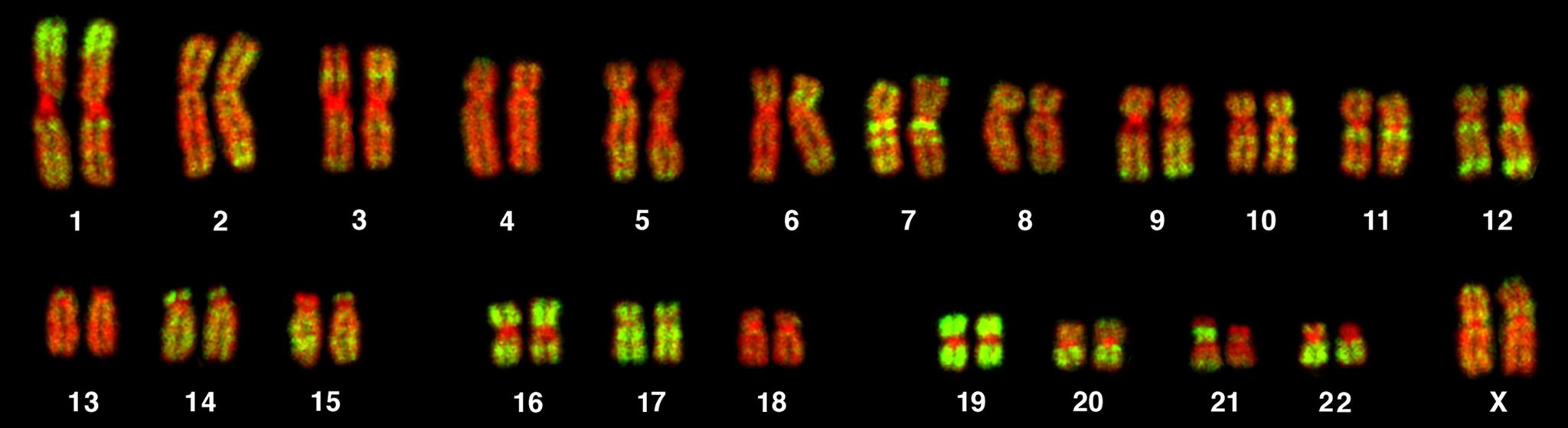
Image: Bolzer et al. PLoS Biol 3(5): e157 DOI: 10.1371/journal.pbio.0030157
Mutations of tumour suppressor genes
Some genetic change is dominant at the cellular level in that only one allele is required to be mutated for an effect to be seen. By contrast, tumour suppressor genes are recessive at the cellular level. This means both alleles (one on the paternal and the other on the maternal chromosome) need to be inactivated for an effect to be seen i.e. two ‘hits’ have to occur.
Although both changes (two hits) can occur due to UVR damage, it is possible to inherit a mutation on one allele and for the second genetic change (‘hit’) to occur due to UVR at a later time on the other allele. This is known as the Knudson two hit hypothesis which states that if a person inherits a germline mutation in a tumour suppressor gene in an autosomal dominated pattern, tumours will occur at a younger age due to only one more hit being required to advance to the next stage of carcinogenesis. It is also implicit in this model, that the chance of one individual acquiring multiple primary tumours if they have inherited a germline mutation, is also increased. In some cases involving the skin, a single patient might have hundreds or rarely even thousands of skin cancers.
The practical point is that some inherited syndromes involving tumour suppressor genes may lead to some types of skin cancer, and that:
- these follow an autosomal pattern of inheritance within the kindred
- there may be multiple primary tumours
- tumours occur at a young age
Some cases of melanoma are familial and are due to mutations in tumour suppressor genes (OMIM #600160), as are some cases of basal cell carcinoma (so called Basal Cell Nevus Syndrome also known as Gorlin’s syndrome, OMIM #109400). We will discuss the clinical aspect of these syndromes later in skincancer909.
Genetics: complex
Finally, although I have not specifically mentioned it explicitly, skin cancer susceptibility is also genetically complex. The degree of melanin pigmentation is a major risk factor, and variation is skin colour reflects the effects of a large number of genes (hence complex). Everyday common sense tells us that skin colour variation is under genetic control, but that it does not follow a Mendelian pattern of inheritance.
There are other traits that likely influence skin cancer susceptibility, although they have been less well studied. We know for instance that there are modest differences in DNA repair between people, likely the result of variation at some of the genes that code for enzymes involved in UVR induced DNA damage. There may well be other factors not yet discovered, too.
Skin cancer: more than the accumulation of mutations
The theme I have used to explain skin cancer is that the accumulation of mutations leads to the cancer phenotype, and than anything that increases DNA damage (such as pale skin) will increase cancer rates. There is however one important bit of the skin cancer jigsaw that this model is missing: the role of the immune system.
The skin is an immunological organ, acting both in a sensory capacity, and as an effector wing (i.e. as a target). The epidermis contains Langerhans’ cells — professional antigen presenting cells — and the dermis contains many other immunological cells, including antigen presenting cells. In addition the epidermis contains occasional T cells. Although the mechanistic details are unclear, the critical role of the immune system in human skin cancer, is demonstrated from clinical observations of what happens to patients who receive organ transplants or who are immunosuppressed for other reasons.
Increased rates of skin cancer in organ transplant recipients
Patients who have undergone allogeneic organ transplants (such as heart, liver or kidney) usually require lifelong immunosuppression to suppress donor organ rejection. Soon after the development of renal transplantation, it became clear that the rates of the common non-melanoma skin cancers, particularly squamous cell carcinoma, were greatly increased.
This increased risk is secondary to the immunosuppression these patients receive, but in addition there is a further factor: some immunosuppressive drugs such as azathioprine directly increase UVR induced DNA damage. For clarity, I will state that the increased cancer risk is seen in immunosuppressed patients who are not taking azathioprine; and that the increased cancer rates are also seen in people who are immunosuppressed for reasons unrelated to organ transplantation.
By Tiiu Sild – Own work, Public Domain, Link. Reconstruction of Dr Barnard’s first human heart transplantation in December 1967
The exact mechanism or mechanisms by which immunosuppression increases skin cancer rates is unclear. One possibility is that immunosuppression might allow certain oncogenic viruses to play a causal role. For instance, organ transplant recipients are at increased risk of cervical and anal cancer, cancers that are caused by oncogenic subtypes of human papilloma viruses (HPV16 & HPV18). Other HPV types can infect skin and cause common viral warts, and indeed some immunosuppressed patients suffer from a high prevalence of common viral warts. However, the HPVs that are known to be oncogenic at other body sites, are not implicated in skin cancers.
By contrast a rare skin cancer, Merkel Cell Carcinoma (MCC), is associated with a viral infection with the Merkel Cell Polyomavirus, and the virus is thought to play a causal role in the development of this cancer (MCC is rare and is dealt with in the Rare Skin Cancer chapter).
Another possibility, involving a mechanism that is better understood in the mouse, is that immune surveillance plays a role. It is widely believed — and there is increasing evidence in man for this view — that the immune system acts against cancerous clones, and is able to recognise them as ‘foreign’, and remove them. In this scenario, suppression of the immune system impairs this anti-tumour immunosurveillance, leading to an increase in skin cancer rates.
Questions: Bench to clinic
- Which areas of skin receive the most UVR?
- How — and why— is ageing related to skin cancer risk?
- Why might global warming increase skin cancer rates in some populations ?
- What is meant by sun-sensitive?
- What are the clinical features of sun-sensitivity?
- What does the melanocortin-1 receptor (MC1R) control?
- Why are mutations of some genes recessive at the cellular level, but show a dominant pattern of inheritance in families?
- Why do patients with the Basal Cell Nevus syndrome present at a young age?
- Name two reasons that some patients with organ transplants have an elevated risk of some skin cancers.
- Why is the mechanistic relation between some viruses and some skin cancers problematic?
A PDF containing the above questions and the answers is here. The video talkover below goes through the questions and answers in greater depth.
Skincancer909 by Jonathan Rees is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Where different rights apply for any figures, this is indicated in the text.